By Carter Dewees
For the Birmingham Times
Day in and day out, doctors, nurses, and essential workers tend to patients and save lives. Over the past year, in particular, these everyday heroes have been on the job 12 to 15 hours a day—sometimes without time off—which has meant a seismic change in both their professional and personal lives.
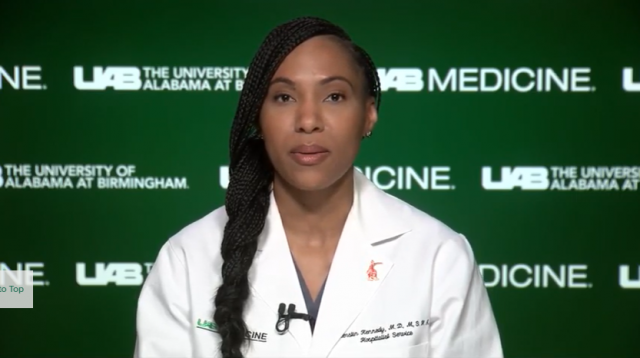
For Kierstin Kennedy, M.D., associate professor and chief of hospital medicine at the University of Alabama at Birmingham (UAB), that meant a greater appreciation of resources when the hospital began to run short of supplies, such as hand sanitizer and sanitizing wipes.
With this month the one-year anniversary of COVID-19, The Birmingham Times asked Kennedy to reflect on the past year from both professional and personal perspectives and share lessons she learned.
The Birmingham Times: How has the COVID-19 pandemic affected you?
Dr. Kennedy: “It has been a whirlwind. I mean we were not prepared for this, and not just from a medical standpoint, obviously, because we had not seen this virus. We didn’t know how to treat it and how it was going to behave. We weren’t necessarily prepared on the home front, either, you know, [because we were unaware of] just how it was going to affect us while trying to balance our personal lives and work. So, it’s definitely been a really overwhelming time.
“The other thing that’s been very surprising for me is that we did not anticipate that COVID-19 would become such a politically charged, controversial topic. I will say, as a physician, it’s been very shocking for me. I’m just not used to having to argue with people about the validity of a disease. … I’ve never had anyone tell me the flu isn’t real. … It’s been a very sort of surreal experience from that standpoint, and there’s no training for that in medical school.”

How has the COVID-19 pandemic changed you?
“It has certainly made me more patient. I think it has made me a lot more appreciative of resources, too, because there was a period during the pandemic when we didn’t know if we would have enough masks. We would meet every morning to go over our supply of hand sanitizer and sanitizing wipes, things we’ve always had in surplus that we never thought about. Suddenly, we were trying to figure out how to ration, reuse, or sanitize things on our own. So, it definitely gave me a greater appreciation for the resources we have
“Also, I think it’s made me a little more focused on public health in a way that I hadn’t been previously. … That’s not my background, … but suddenly I found myself as an inpatient doctor trying to help educate the public about this illness because I see it from a perspective that other people are not able to see it from. The outpatient doctors who have a little more experience in matters as it relates to public health aren’t taking care of patients that are sick in the hospital, so some of us have had to step outside the walls of the hospital. … In that regard, I think it’s been nice because I’ve had to develop a new skill set—and that’s always good for you.”
What would you say to those who haven’t taken this seriously?
“When you look at the death toll [in the U.S.] at this point, it’s over 500,000, which is pretty close to the death toll for cancer. We don’t say that people concerned about cancer are overreacting. … I think we should be beyond the point of arguing about whether or not [COVID-19] is real. I’m seeing people in the hospital by themselves, surrounded by strangers, unable to breathe, terrified of what’s going to happen next, seeing people die. Then I walk outside and see people at restaurants, people hanging out; … I go on Facebook, and people are saying [the virus] is not real. … There’s a dichotomy between what we were seeing [in hospitals] for a period of time—when we didn’t have adequate resources, when we didn’t have enough beds, … [when] we were trying to stabilize patients that needed to go to the [intensive care unit (ICU)] while we tried to create another ICU or, literally, turned the recovery part of an [operating room (OR )] into an ICU—and what feels like a war zone outside, where people make fun of [the virus].”



